3 Reasons I Do Not Recommend a Vegetarian or Vegan Diet - Seattle Nutrition Blog
f insulin resistance is primarily caused and perpetuated by a carbohydrate-rich diet, consider this: You cannot reach optimal dietary protein goals from a vegan or vegetarian diet without also consuming mountains of starchy carbohydrates and loads of extra calories.
My clients often require a daily protein intake of about 100g (depending on the individual’s body size, activity, and digestive health). This breaks down to roughly 30-35g of protein per meal.
You would have to consume 4 cups of cooked quinoa to meet that requirement for one meal.
My Clients Get Better Results with Animal Proteins
When women come to me with symptoms like sleep issues, sugar cravings, and irregular periods or a PCOS diagnosis, my first thought is adrenal fatigue. Adrenal symptoms like these are often paired with prolonged chronic stress, blood sugar dysregulation, and insulin resistance.
Which leads me to the question - are these women getting enough quality protein? In an effort to marry two articles I’ve previously written on the role of protein in insulin resistance, and the health effects of a vegan diet, I’m bringing these two ideas together to help you see the full picture.
Hi darlings. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress, insulin resistance, and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between their lab values and what their body is saying. Before you continue, click here to read my Medical Disclaimer.
In this article, you’ll learn:
what is insulin resistance?
why protein matters
why I won’t work with clients who are unwilling to include animal proteins in their diet
what is insulin resistance?
In short, glucose is the molecular form of sugar that is used to create energy within the mitochondria of cells in the form of ATP, or Adenosine TriPhosphate. Glucose is broken down from all types of carbohydrates, including starchy vegetables, legumes, grains, and yes, sugars.
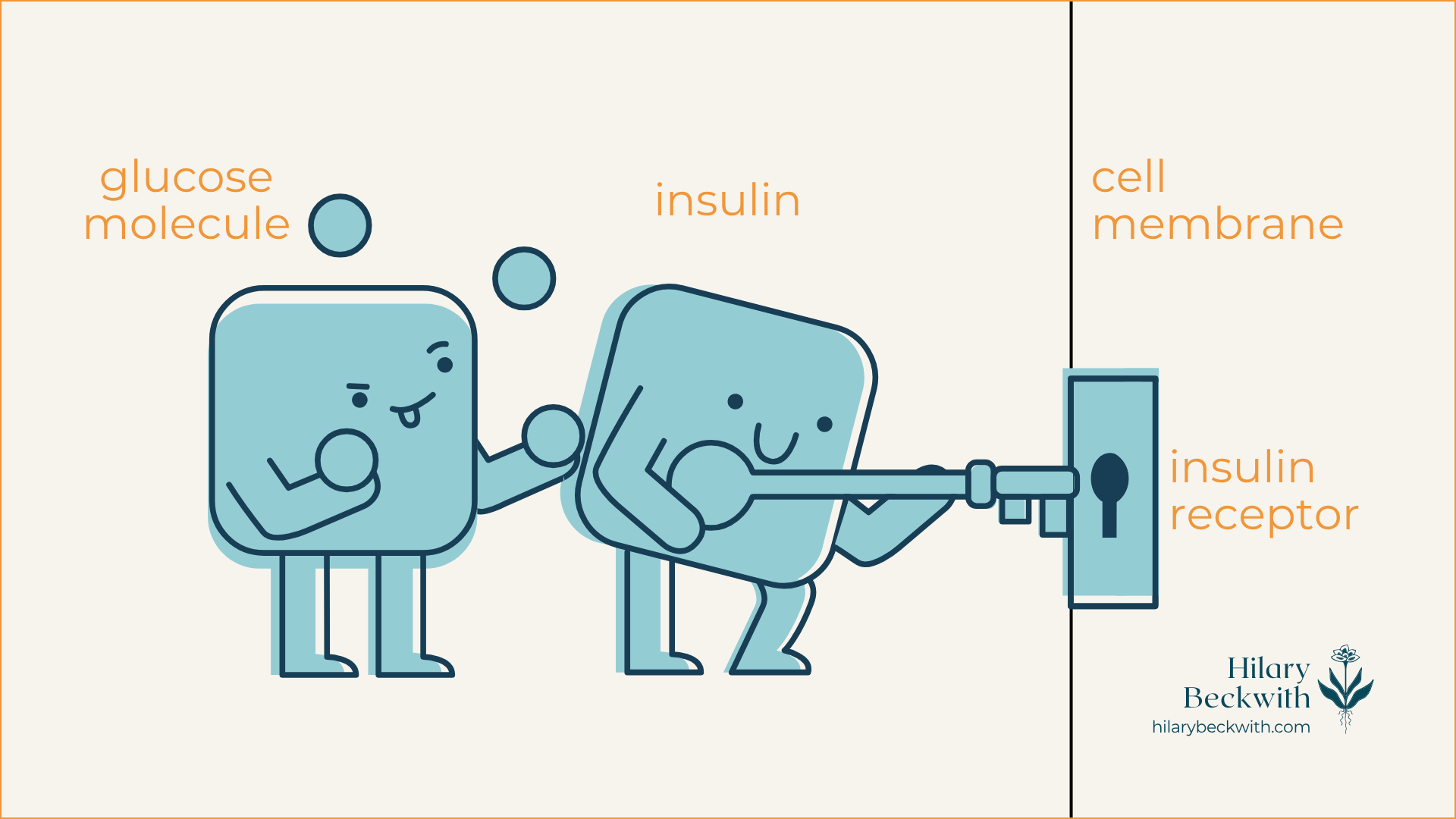
When dietary carbohydrates are broken down into glucose, insulin from the pancreas acts as a key-holder that unlocks the door to the cell (insulin receptor) and shuttles glucose in for energy production. Once cells have had their fill, the remaining glucose is converted into stored forms of glucose and stored in the liver and fat tissue.
For someone who regularly consumes carbohydrate-rich meals and snacks, there is often more glucose in their bloodstream than cells can handle. This causes cells to deactivate their insulin receptors, sending the message, “we’ve had enough!”.
This deactivation of insulin receptors is known as insulin resistance, and it becomes a problem that perpetuates itself until meaningful dietary and lifestyle changes are made.
why protein matters
Dietary protein is essential to many biological functions. It’s needed for nutrient transport across cell membranes, used in the formation of antibodies, needed for neurotransmitter formation which impacts mood and sleep, and it’s needed to strengthen muscles.
Most of us don’t get enough protein daily. In fact the current Recommended Dietary Allowance (RDA) for protein was decided in 1989, and is considered the minimum needed to maintain health in sedentary individuals [1], not what is best for optimal health and activity levels. The RDA for protein is 0.75g per 1kg of body weight.
For a female-bodied individual weighing 150lbs (68kg), the RDA is 51g protein daily. More current research has found that higher protein intake is more conducive to optimal health and should be considered over the current RDA [2}.
If you are the person whose shelves are loaded with “protein-packed” packaged snacks, vegan protein powders, or if you came here searching for vegetarian high-protein recipes, consider this: Plant proteins and animal proteins are not equally absorbed and used by human bodies [3].
Don’t take my word for it - read the research for yourself.
HERE’S WHERE IT CAN GO WRONG
If insulin resistance is primarily caused and perpetuated by a carbohydrate-rich diet, consider this: You cannot reach optimal dietary protein goals from a vegan or vegetarian diet without also consuming mountains of starchy carbohydrates and loads of extra calories.
My clients often require a daily protein intake of about 100g (depending on the individual’s body size, activity, and digestive health). This breaks down to roughly 30-35g of protein per meal.
You would have to consume 4 cups of cooked quinoa to meet that requirement for one meal.
Here are some additional protein source comparisons:
2 cans chickpeas (drained) = 704 calories + 36g protein
3/4 block tofu = 266 calories + 31.8g protein
4 cups cooked quinoa = 888 calories + 32.8g protein
4oz grass-fed beef = 157 calories + 24g protein (plus grass-fed beef is shown to have a more dense nutrient profile than conventional beef, including significantly higher levels of superoxide dismutase and Omega 3 fatty acids)
1/2 fillet wild-caught salmon = 209 calories + 31g protein
5 large eggs = 360 calories + 31.5g protein
1 chicken breast (120g) = 198 calories + 37g protein
This lack of protein, paired with carbohydrate-rich eating habits is also a major driver of pathogenic infections, such as candida or yeast overgrowth, small intestinal bacterial overgrowth (SIBO), and can impair digestive function over time, increasing susceptibility for parasite and helicobacter pylori infections as well. I’ll explain more of this mechanism later in the post.
why i don’t work with clients who are unwilling to consume animal proteins
The short answer - their success and my reputation depend on it.
I have worked with clients in the past who prefer vegetarian and vegan diets, and the reality is - they do not celebrate the same successes that my omnivorous clients do when it comes to resolving their digestive symptoms, PCOS symptoms, and weight issues.
If that sounds too harsh, please know that I do hold space for different views on vegetarian vs vegan vs omnivorous diets, and can appreciate that there are many different reasons for choosing one over another.
This decision does not come from a place of judgment, but rather for the sake of the long-term health and success of the women who come to see me.
When it comes to symptoms of hormone imbalance, sleep issues, blood sugar management issues, weight loss, and irregular periods, a diet without animal proteins simply will not support their efforts to address symptoms.
Here’s where I see the biggest impacts.
HORMONE HEALTH
The women and female-bodied individuals who come to see me, often present with symptoms of hormone imbalance, be it a PCOS diagnosis, irregular periods, PMS symptoms, painful periods, mood and sleep disruptions around their periods, migraines around their periods, and weight gain in their belly or hips.
Aside from the obvious ovaries, hormones are largely modulated by the adrenal glands and the liver. The adrenal glands are responsible for producing any sex hormones that are not produced by the ovaries or testes, and the liver is charged with hormone balance, in that, it is responsible for deactivating and eliminating excess hormones to maintain balance.
A diet rich in carbohydrates, and especially low in protein, drives insulin resistance which disrupts the HPA (hypothalamus, pituitary, adrenal) axis and consequently, the ability of the ovaries and adrenal glands to produce hormones.
Additionally, when left unaddressed, this disruption leads to prolonged chronic stress, leading to adrenal fatigue, chronic inflammation, and abnormal thyroid labs. This is a highly complex topic that I go into more detail about here.
Finally, a liver that is overburdened with the job of constantly having to convert excess glucose into fat and glycogen may not be able to effectively metabolize and eliminate excess hormones well, exacerbating hormone imbalance symptoms.
BLOOD SUGAR BALANCE
If you wake up around 2:00 am most nights to pee, or get “hangry” between meals, you have blood sugar regulation issues. This, too, involves your liver and adrenal glands, and is highly driven by a carbohydrate-rich diet, among other things.
Additionally, carb and sugar cravings are common symptoms of the pathogenic infections we discussed earlier. You see, yeast and bacteria LOVE sugar, and when they infiltrate your gut, they live off of your resources. This perpetuates blood sugar imbalances, leading to insulin resistance, adrenal fatigue, and symptoms of hormone imbalance. (seeing a pattern here?)
GUT HEALTH
This topic is multifaceted, but here are the two main points I want to focus on for the sake of this post:
lack of protein inhibits digestion - Healthy digestion relies on many components - a regulated nervous system, optimal output of digestive juices (enzymes and stomach acid), and adequate chewing and mechanical digestion. Consuming protein tells your body to produce stomach acid (HCl) and proteolytic enzymes. With a low-protein diet, HCl production suffers, and so does your digestion. Since one of the main roles of HCl is to disinfect your food, poor HCl output leaves you more susceptible to pathogenic infections of the gut, driving inflammation, hormone issues, and overall discomfort.
migrating motor complex (MMC) - This important mechanism occurs only in a fasted state, and consists of a cascade of events intended to sweep out unwanted microbes from the small intestine. A carbohydrate-rich diet often makes one hungry more frequently throughout the day, leaving very little fasted time for the MMC to activate. If you are one who snacks or grazes throughout the day, you are doing your gut a disservice.
learn something new?
Please share your thoughts and questions in the comments below.
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
National Research Council (US) Subcommittee on the Tenth Edition of the Recommended Dietary Allowances. “Protein and Amino Acids.” Recommended Dietary Allowances: 10th Edition., U.S. National Library of Medicine, 1 Jan. 1989, www.ncbi.nlm.nih.gov/books/NBK234922/.
Hudson, Joshua L, et al. “Protein Intake Greater than the RDA Differentially Influences Whole-Body Lean Mass Responses to Purposeful Catabolic and Anabolic Stressors: A Systematic Review and Meta-Analysis.” Advances in Nutrition (Bethesda, Md.), U.S. National Library of Medicine, 1 May 2020, pmc.ncbi.nlm.nih.gov/articles/PMC7231581/.
Association of Major Dietary Protein Sources with All‐cause and Cause‐specific Mortality: Prospective Cohort Study | Journal of the American Heart Association, www.ahajournals.org/doi/10.1161/JAHA.119.015553. Accessed 3 Oct. 2025.
Treating PCOS with Nutrition: Why Addressing Gut Health is Key
I was once diagnosed with PCOS, and so whenever I am studying it, or hear that someone I know is dealing with it, I light up! It's such an interesting topic to me, and has impacted my life on a deeply emotional level. It’s important to me that you know that I GET IT. More deeply than most, I am right there with you.
For those unfamiliar with the term, PCOS stands for Poly Cystic Ovary Syndrome. It occurs when our body, for whatever reason (more on that later), cannot fully ovulate, meaning, the egg cannot fully break through the follicle wall and ovary wall into the fallopian tube. Instead, the egg remains in the ovary wall and creates a cyst. When this happens repeatedly, the ovary becomes covered in cysts.
PCOS Symptoms
This is an exciting topic for me. (Nerd alert!)
But for real - I was once diagnosed with PCOS, and so whenever I am studying it, or hear that someone I know is dealing with it, I light up! It's such an interesting topic to me, and has impacted my life on a deeply emotional level.
It’s important to me that you know that I GET IT. More deeply than most, I am right there with you.
For those unfamiliar with the term, PCOS stands for PolyCystic Ovary Syndrome. It occurs when our body, for whatever reason (more on that later), cannot fully ovulate, meaning the egg cannot fully break through the follicle wall and ovary wall into the fallopian tube. Instead, the egg remains in the ovary wall and creates a cyst. When this happens repeatedly, the ovary becomes covered in cysts.
The really heartbreaking part is that female-bodied individuals who've been diagnosed with PCOS are often diagnosed while in the process of trying to get pregnant.
But why aren't our health care professionals looking into this when we come to them earlier on, with PCOS symptoms of irregular periods, cystic acne, blood sugar issues, weight gain or PCOS belly, and even chronic pain...
Why do they just throw 'the pill' at us instead of investigating the root cause?
Why do we have to wait until the moment we are in a super vulnerable stage (anyone who's ridden the roller coaster of trying to conceive...), when we could have addressed it sooner?!
This, to me, is truly maddening.
The most important takeaway from this post: PCOS is not an ovarian issue - it is a GUT issue. Addressing gut health will go a long way to improving PCOS symptoms.
what are PCOS symptoms?
If you have been given a PCOS diagnosis and have been advised to seek infertility treatments, know that you have other options. PCOS treatment does not involve petri dishes, hormone shots, egg extraction, etc..
If PCOS is the causal factor in your infertility, it can be addressed dietarily, without the use of expensive infertility treatments.
PCOS IS NOT AN OVARIAN CONDITION - IT IS A GUT ISSUE.
Whether or not you are trying to get pregnant, are done having kids, or don't want kids - if you are a female-bodied person, then you, or someone you know, will probably encounter PCOS symptoms at some point.
Before we really dig in, I want to briefly share my story as it relates to PCOS.
my PCOS story
I was a "late bloomer" (first red flag), did not get my first period until I was 16 or 17. They were irregular from the start and for decades after.
Add to that, I was pretty ignorant of how my body was supposed to function, due to my parents' religious beliefs and consequently a severe disconnection from my body’s needs.
(Um, side note: Can we PLEASE normalize talking to kids about their bodies?!)
Cystic acne from my teen years and many years into adulthood, I have always had excess belly and hip fat (commonly known as PCOS belly), difficulty losing weight, symptoms of low blood sugar, the works.
When I was 18 (ca. 2000) and my periods had still not regulated, I got my first gynecological exam. I was given a prescription for 'the pill' and was told that it would regulate my cycle (and it did).
I didn’t know what I didn’t know. I trusted that my doctor knew what was best. I didn’t understand until later that if that doctor had taken the time to help me find the root causes of my PCOS symptoms, I would have been spared decades of heartache and confusion.
Fast forward to 2009, my partner and I decided we wanted children, so I stopped the pill, and we began trying to conceive. It was a few months without a period that we started to get concerned.
My GYN ordered an ultrasound, and I was diagnosed with PCOS.
The GYN prescribed Clomid (my apologies to anyone who had to encounter me during this time). Clomid is a medication that stimulates an increase in hormones involved in ovulation.
When two rounds of Clomid were unsuccessful, we were left with the decision to come up with the money to pursue infertility treatment or to just keep our fingers crossed.
We left that appointment with broken hearts, as that kind of money was truly foreign to us at the time.
The short story is, we never did have children (and are now very happy with our lifestyle without children). We tried for many years before finally making a very intentional decision to NOT have children.
Being a holistic healthcare provider now has taught me a lot about my PCOS diagnosis and how to address them. And although I no longer want children of my own, I no longer have signs of PCOS symptoms!
PCOS treatment
PCOS occurs when there is an imbalance of hormones. Period.
This imbalance can be caused by a number of things: Pituitary dysfunction, adrenal dysfunction, toxic overload, liver dysfunction...
It often (not always) has very little to do with the ovaries themselves.
PCOS is the end result of other dysfunctions in the body, and symptoms of PCOS can, and often do, make it difficult for a female to get pregnant.
Here’s a brief breakdown of the female reproductive system as it relates to PCOS symptom. For those who want a more thorough explanation, read this article.
Remember that this system requires our brain (hypothalamus) to communicate with the pituitary gland, which releases hormones to stimulate egg growth, which increases estrogen production, and once the egg matures and breaks through the ovary wall, then progesterone is produced. From there, we need our liver to detoxify the excess hormones that are now circulating throughout our body (yes, these hormones need a way out!).
Because other systems in our body use similar pathways, it is easy to create bottlenecks of dysfunction.
The most obvious example as it relates to PCOS symptoms, is blood sugar regulation. You might remember from an article I wrote recently in regards to blood sugar balance, that it is not just about what you eat. It, too, requires your hypothalamus to communicate with your pituitary gland, telling it to produce hormones, that travel to your adrenal glands, telling them to produce other hormones (epinephrine and cortisol), that stimulate the pancreas to release OTHER hormones.... (you get the idea).
When we are chronically stressed (meaning, our body produces cortisol more frequently than it needs to), or we overly consume sugar, processed foods, or medications, we create dysfunction in other systems of our body.
THE GOOD NEWS IS…
Unless your body has an underlying dysfunction within your individual chemical makeup, all of these things can be addressed using dietary and lifestyle changes.
And for those of you who have been told PCOS is the cause of your infertility, knowing this is life-changing.
Effective treatment of PCOS symptoms starts by looking at the root cause. Here’s what individualized PCOS treatment means for you:
reduce PCOS belly, or weight loss in the belly/hips
regulate menstrual cycles
improve ovulation cycle
improve insulin sensitivity
prevent Type II Diabetes
improve skin clarity
Individualized assessments and a customized care plan based on your body’s unique health needs are essential to getting relief from your PCOS symptoms. Anything else is just throwing spaghetti at the wall, and aren’t you tired of doing this?
That being said, there are ways to effectively support common PCOS symptoms with more foundational recommendations.
how to get rid of PCOS
Eat whole foods. Ditch anything that strays from its whole form in any way, as much as possible. Processed foods, and especially refined carbohydrates, lead to inflammatory conditions such as leaky gut, in addition to promoting insulin resistance.
Stop counting calories. You are not doing your body any favors by restricting how many calories are consumed. This is a temptation for many female-bodied individuals, especially because excess weight is often harder to shed with PCOS. The quality of food you consume carries more value than the amount of calories, in regards to hormone balance.
Regulate your blood sugar (here is a great article on how to do that). For many, it involves eating more quality fats & proteins each meal, increasing (whole) fiber, and decreasing the amount of starchy foods, grains, and sugars/sweeteners (yes, even 'low calorie'). Not only will this help your PCOS symptoms, you'll also get less "hangry" symptoms (your friends & family will thank you!)
Stop snacking. Eating more quality fats/proteins and fiber each meal will likely help you feel more satiated (satisfied) and not want to snack anyways. However, a conscious effort to not snack will help improve insulin sensitivity, which will support your adrenal glands and liver function.
supplements to improve PCOS symptoms
**Always consult with a trusted health care practitioner before adding any supplements to your regimen. Additionally, taking supplements without addressing foundational factors (discussed above) is a waste of your money. Click here to read my full Medical Disclaimer.
Myo-Inositol Plus (Bioclinic Naturals)- improves insulin response, and can help lower excess estrogens & testosterone.
HPA Adapt (Integrative Therapeutics)- supports the cohesion of the Hypothalamus, Pituitary, & Adrenal (HPA) axis
Calcium D-Glucarate (Integrative Therapeutics)- Supports the specific detox pathway, called glucuronidation, in the liver needed to deactivate and remove excess hormones, like estrogen and testosterone.
BroccoProtect (Designs for Health)- supports Phase II detox pathways in the liver. Females with PCOS often have sluggish Phase II detox pathways, and BroccoProtect helps to support these pathways to ensure the deactivation and removal of excess hormones.
Megaspore Probiotics (Microbiome Labs)- Introducing a good quality probiotic to support the elimination of excess hormones after they've been neutralized by the liver, is essential to making sure they don't get reabsorbed into your body. Elimination is key!
was this helpful?
What’s your PCOS story?
Share your thoughts on PCOS in the comments below, and help another PCOS warrior feel less alone.
NUTRITION SERVICES
ADDITIONAL RESOURCES