3 Reasons I Do Not Recommend a Vegetarian or Vegan Diet - Seattle Nutrition Blog
My Clients Get Better Results with Animal Proteins
When women come to me with symptoms like sleep issues, sugar cravings, and irregular periods or a PCOS diagnosis, my first thought is adrenal fatigue. Adrenal symptoms like these are often paired with prolonged chronic stress, blood sugar dysregulation, and insulin resistance.
Which leads me to the question - are these women getting enough quality protein? In an effort to marry two articles I’ve previously written on the role of protein in insulin resistance, and the health effects of a vegan diet, I’m bringing these two ideas together to help you see the full picture.
Hi darlings. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress, insulin resistance, and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between their lab values and what their body is saying. Before you continue, click here to read my Medical Disclaimer.
In this article, you’ll learn:
what is insulin resistance?
why protein matters
why I won’t work with clients who are unwilling to include animal proteins in their diet
what is insulin resistance?
In short, glucose is the molecular form of sugar that is used to create energy within the mitochondria of cells in the form of ATP, or Adenosine TriPhosphate. Glucose is broken down from all types of carbohydrates, including starchy vegetables, legumes, grains, and yes, sugars.
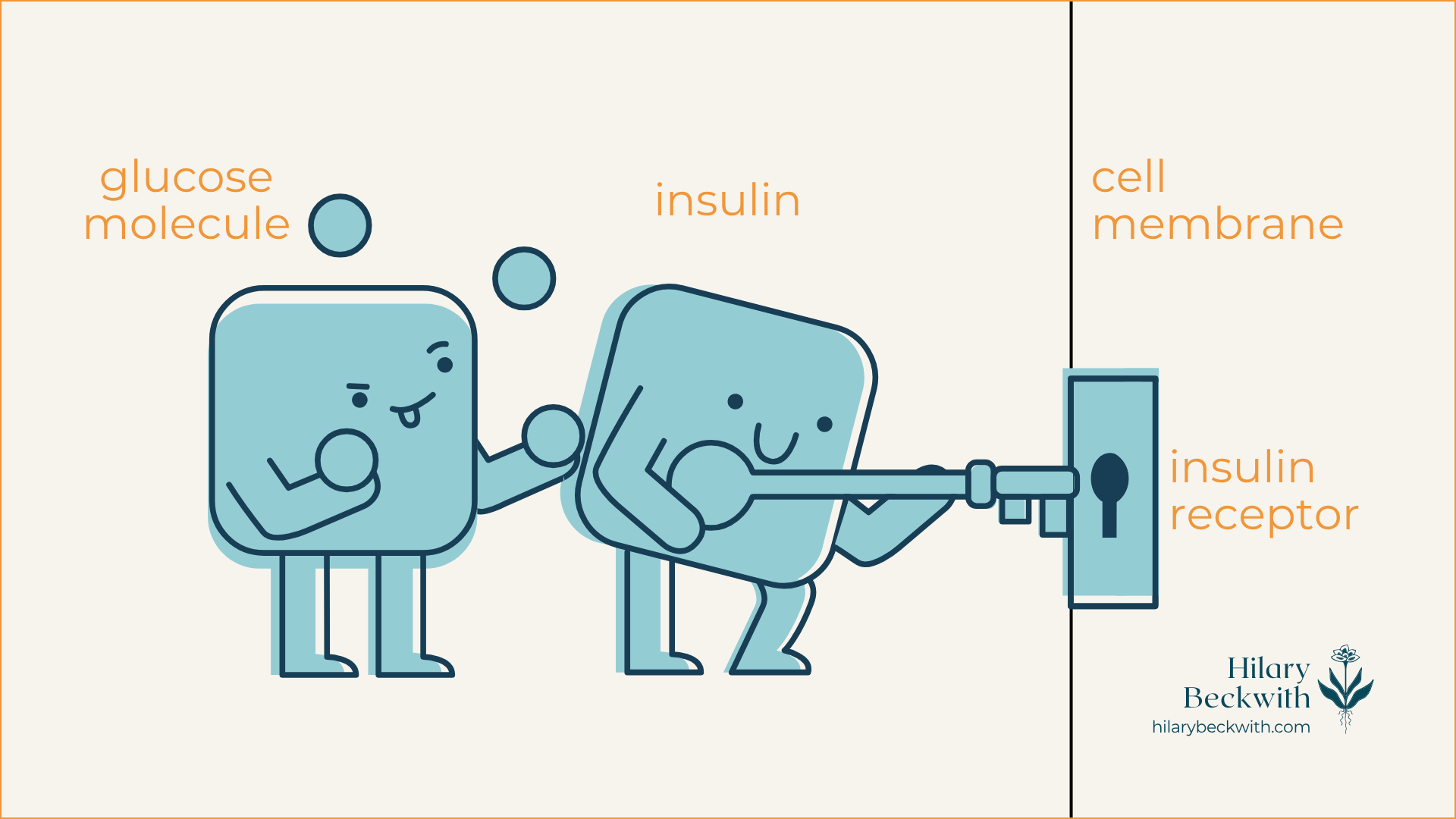
When dietary carbohydrates are broken down into glucose, insulin from the pancreas acts as a key-holder that unlocks the door to the cell (insulin receptor) and shuttles glucose in for energy production. Once cells have had their fill, the remaining glucose is converted into stored forms of glucose and stored in the liver and fat tissue.
For someone who regularly consumes carbohydrate-rich meals and snacks, there is often more glucose in their bloodstream than cells can handle. This causes cells to deactivate their insulin receptors, sending the message, “we’ve had enough!”.
This deactivation of insulin receptors is known as insulin resistance, and it becomes a problem that perpetuates itself until meaningful dietary and lifestyle changes are made.
why protein matters
Dietary protein is essential to many biological functions. It’s needed for nutrient transport across cell membranes, used in the formation of antibodies, needed for neurotransmitter formation which impacts mood and sleep, and it’s needed to strengthen muscles.
Most of us don’t get enough protein daily. In fact the current Recommended Dietary Allowance (RDA) for protein was decided in 1989, and is considered the minimum needed to maintain health in sedentary individuals [1], not what is best for optimal health and activity levels. The RDA for protein is 0.75g per 1kg of body weight.
For a female-bodied individual weighing 150lbs (68kg), the RDA is 51g protein daily. More current research has found that higher protein intake is more conducive to optimal health and should be considered over the current RDA [2}.
If you are the person whose shelves are loaded with “protein-packed” packaged snacks, vegan protein powders, or if you came here searching for vegetarian high-protein recipes, consider this: Plant proteins and animal proteins are not equally absorbed and used by human bodies [3].
Don’t take my word for it - read the research for yourself.
HERE’S WHERE IT CAN GO WRONG
If insulin resistance is primarily caused and perpetuated by a carbohydrate-rich diet, consider this: You cannot reach optimal dietary protein goals from a vegan or vegetarian diet without also consuming mountains of starchy carbohydrates and loads of extra calories.
My clients often require a daily protein intake of about 100g (depending on the individual’s body size, activity, and digestive health). This breaks down to roughly 30-35g of protein per meal.
You would have to consume 4 cups of cooked quinoa to meet that requirement for one meal.
Here are some additional protein source comparisons:
2 cans chickpeas (drained) = 704 calories + 36g protein
3/4 block tofu = 266 calories + 31.8g protein
4 cups cooked quinoa = 888 calories + 32.8g protein
4oz grass-fed beef = 157 calories + 24g protein (plus grass-fed beef is shown to have a more dense nutrient profile than conventional beef, including significantly higher levels of superoxide dismutase and Omega 3 fatty acids)
1/2 fillet wild-caught salmon = 209 calories + 31g protein
5 large eggs = 360 calories + 31.5g protein
1 chicken breast (120g) = 198 calories + 37g protein
This lack of protein, paired with carbohydrate-rich eating habits is also a major driver of pathogenic infections, such as candida or yeast overgrowth, small intestinal bacterial overgrowth (SIBO), and can impair digestive function over time, increasing susceptibility for parasite and helicobacter pylori infections as well. I’ll explain more of this mechanism later in the post.
why i don’t work with clients who are unwilling to consume animal proteins
The short answer - their success and my reputation depend on it.
I have worked with clients in the past who prefer vegetarian and vegan diets, and the reality is - they do not celebrate the same successes that my omnivorous clients do when it comes to resolving their digestive symptoms, PCOS symptoms, and weight issues.
If that sounds too harsh, please know that I do hold space for different views on vegetarian vs vegan vs omnivorous diets, and can appreciate that there are many different reasons for choosing one over another.
This decision does not come from a place of judgment, but rather for the sake of the long-term health and success of the women who come to see me.
When it comes to symptoms of hormone imbalance, sleep issues, blood sugar management issues, weight loss, and irregular periods, a diet without animal proteins simply will not support their efforts to address symptoms.
Here’s where I see the biggest impacts.
HORMONE HEALTH
The women and female-bodied individuals who come to see me, often present with symptoms of hormone imbalance, be it a PCOS diagnosis, irregular periods, PMS symptoms, painful periods, mood and sleep disruptions around their periods, migraines around their periods, and weight gain in their belly or hips.
Aside from the obvious ovaries, hormones are largely modulated by the adrenal glands and the liver. The adrenal glands are responsible for producing any sex hormones that are not produced by the ovaries or testes, and the liver is charged with hormone balance, in that, it is responsible for deactivating and eliminating excess hormones to maintain balance.
A diet rich in carbohydrates, and especially low in protein, drives insulin resistance which disrupts the HPA (hypothalamus, pituitary, adrenal) axis and consequently, the ability of the ovaries and adrenal glands to produce hormones.
Additionally, when left unaddressed, this disruption leads to prolonged chronic stress, leading to adrenal fatigue, chronic inflammation, and abnormal thyroid labs. This is a highly complex topic that I go into more detail about here.
Finally, a liver that is overburdened with the job of constantly having to convert excess glucose into fat and glycogen may not be able to effectively metabolize and eliminate excess hormones well, exacerbating hormone imbalance symptoms.
BLOOD SUGAR BALANCE
If you wake up around 2:00 am most nights to pee, or get “hangry” between meals, you have blood sugar regulation issues. This, too, involves your liver and adrenal glands, and is highly driven by a carbohydrate-rich diet, among other things.
Additionally, carb and sugar cravings are common symptoms of the pathogenic infections we discussed earlier. You see, yeast and bacteria LOVE sugar, and when they infiltrate your gut, they live off of your resources. This perpetuates blood sugar imbalances, leading to insulin resistance, adrenal fatigue, and symptoms of hormone imbalance. (seeing a pattern here?)
GUT HEALTH
This topic is multifaceted, but here are the two main points I want to focus on for the sake of this post:
lack of protein inhibits digestion - Healthy digestion relies on many components - a regulated nervous system, optimal output of digestive juices (enzymes and stomach acid), and adequate chewing and mechanical digestion. Consuming protein tells your body to produce stomach acid (HCl) and proteolytic enzymes. With a low-protein diet, HCl production suffers, and so does your digestion. Since one of the main roles of HCl is to disinfect your food, poor HCl output leaves you more susceptible to pathogenic infections of the gut, driving inflammation, hormone issues, and overall discomfort.
migrating motor complex (MMC) - This important mechanism occurs only in a fasted state, and consists of a cascade of events intended to sweep out unwanted microbes from the small intestine. A carbohydrate-rich diet often makes one hungry more frequently throughout the day, leaving very little fasted time for the MMC to activate. If you are one who snacks or grazes throughout the day, you are doing your gut a disservice.
learn something new?
Please share your thoughts and questions in the comments below.
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
National Research Council (US) Subcommittee on the Tenth Edition of the Recommended Dietary Allowances. “Protein and Amino Acids.” Recommended Dietary Allowances: 10th Edition., U.S. National Library of Medicine, 1 Jan. 1989, www.ncbi.nlm.nih.gov/books/NBK234922/.
Hudson, Joshua L, et al. “Protein Intake Greater than the RDA Differentially Influences Whole-Body Lean Mass Responses to Purposeful Catabolic and Anabolic Stressors: A Systematic Review and Meta-Analysis.” Advances in Nutrition (Bethesda, Md.), U.S. National Library of Medicine, 1 May 2020, pmc.ncbi.nlm.nih.gov/articles/PMC7231581/.
Association of Major Dietary Protein Sources with All‐cause and Cause‐specific Mortality: Prospective Cohort Study | Journal of the American Heart Association, www.ahajournals.org/doi/10.1161/JAHA.119.015553. Accessed 3 Oct. 2025.