3 Reasons I Do Not Recommend a Vegetarian or Vegan Diet - Seattle Nutrition Blog
f insulin resistance is primarily caused and perpetuated by a carbohydrate-rich diet, consider this: You cannot reach optimal dietary protein goals from a vegan or vegetarian diet without also consuming mountains of starchy carbohydrates and loads of extra calories.
My clients often require a daily protein intake of about 100g (depending on the individual’s body size, activity, and digestive health). This breaks down to roughly 30-35g of protein per meal.
You would have to consume 4 cups of cooked quinoa to meet that requirement for one meal.
My Clients Get Better Results with Animal Proteins
When women come to me with symptoms like sleep issues, sugar cravings, and irregular periods or a PCOS diagnosis, my first thought is adrenal fatigue. Adrenal symptoms like these are often paired with prolonged chronic stress, blood sugar dysregulation, and insulin resistance.
Which leads me to the question - are these women getting enough quality protein? In an effort to marry two articles I’ve previously written on the role of protein in insulin resistance, and the health effects of a vegan diet, I’m bringing these two ideas together to help you see the full picture.
Hi darlings. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress, insulin resistance, and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between their lab values and what their body is saying. Before you continue, click here to read my Medical Disclaimer.
In this article, you’ll learn:
what is insulin resistance?
why protein matters
why I won’t work with clients who are unwilling to include animal proteins in their diet
what is insulin resistance?
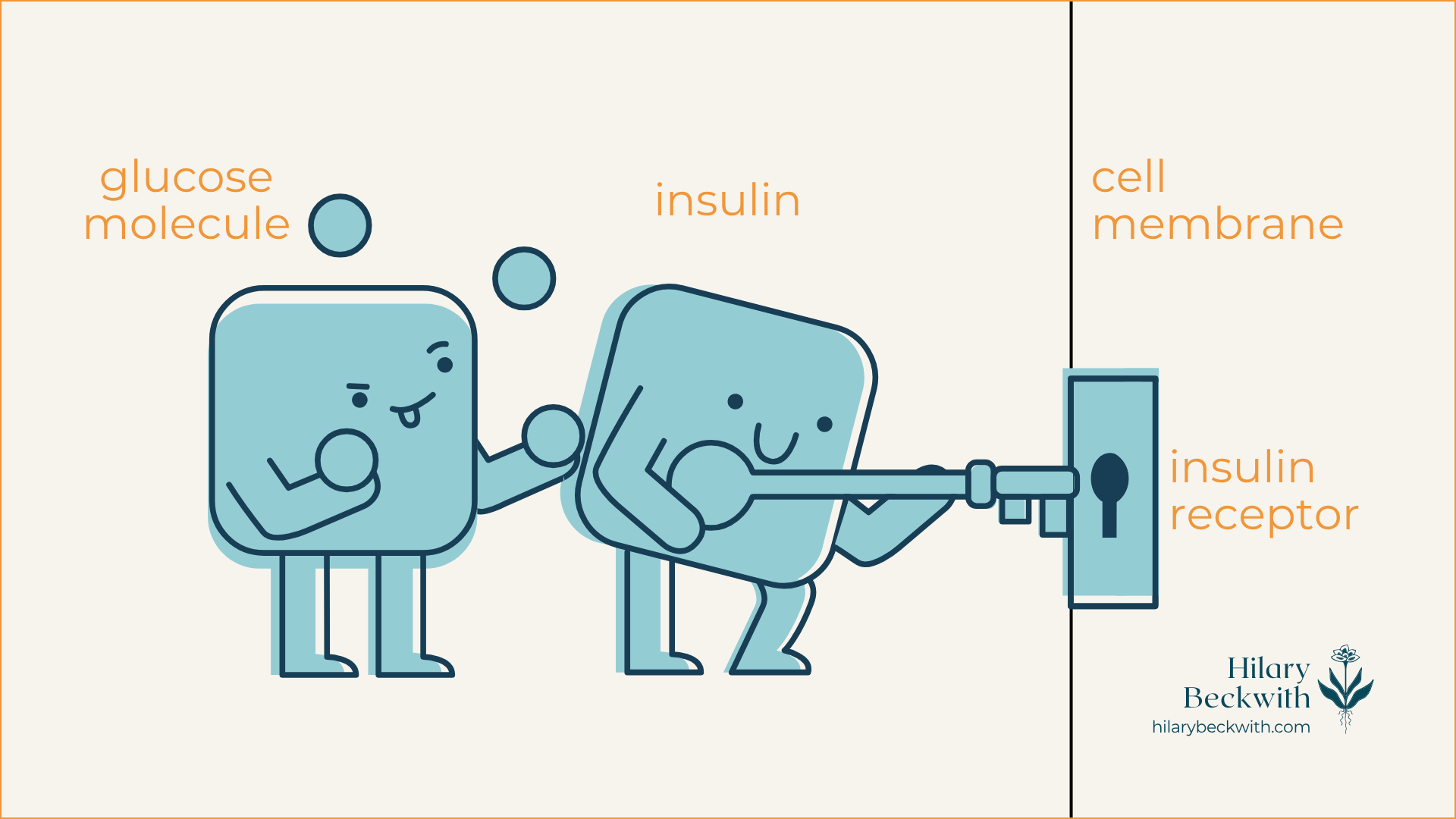
In short, glucose is the molecular form of sugar that is used to create energy within the mitochondria of cells in the form of ATP, or Adenosine TriPhosphate. Glucose is broken down from all types of carbohydrates, including starchy vegetables, legumes, grains, and yes, sugars.
When dietary carbohydrates are broken down into glucose, insulin from the pancreas acts as a key-holder that unlocks the door to the cell (insulin receptor) and shuttles glucose in for energy production. Once cells have had their fill, the remaining glucose is converted into stored forms of glucose and stored in the liver and fat tissue.
For someone who regularly consumes carbohydrate-rich meals and snacks, there is often more glucose in their bloodstream than cells can handle. This causes cells to deactivate their insulin receptors, sending the message, “we’ve had enough!”.
This deactivation of insulin receptors is known as insulin resistance, and it becomes a problem that perpetuates itself until meaningful dietary and lifestyle changes are made.
why protein matters
Dietary protein is essential to many biological functions. It’s needed for nutrient transport across cell membranes, used in the formation of antibodies, needed for neurotransmitter formation which impacts mood and sleep, and it’s needed to strengthen muscles.
Most of us don’t get enough protein daily. In fact the current Recommended Dietary Allowance (RDA) for protein was decided in 1989, and is considered the minimum needed to maintain health in sedentary individuals [1], not what is best for optimal health and activity levels. The RDA for protein is 0.75g per 1kg of body weight.
For a female-bodied individual weighing 150lbs (68kg), the RDA is 51g protein daily. More current research has found that higher protein intake is more conducive to optimal health and should be considered over the current RDA [2}.
If you are the person whose shelves are loaded with “protein-packed” packaged snacks, vegan protein powders, or if you came here searching for vegetarian high-protein recipes, consider this: Plant proteins and animal proteins are not equally absorbed and used by human bodies [3].
Don’t take my word for it - read the research for yourself.
HERE’S WHERE IT CAN GO WRONG
If insulin resistance is primarily caused and perpetuated by a carbohydrate-rich diet, consider this: You cannot reach optimal dietary protein goals from a vegan or vegetarian diet without also consuming mountains of starchy carbohydrates and loads of extra calories.
My clients often require a daily protein intake of about 100g (depending on the individual’s body size, activity, and digestive health). This breaks down to roughly 30-35g of protein per meal.
You would have to consume 4 cups of cooked quinoa to meet that requirement for one meal.
Here are some additional protein source comparisons:
2 cans chickpeas (drained) = 704 calories + 36g protein
3/4 block tofu = 266 calories + 31.8g protein
4 cups cooked quinoa = 888 calories + 32.8g protein
4oz grass-fed beef = 157 calories + 24g protein (plus grass-fed beef is shown to have a more dense nutrient profile than conventional beef, including significantly higher levels of superoxide dismutase and Omega 3 fatty acids)
1/2 fillet wild-caught salmon = 209 calories + 31g protein
5 large eggs = 360 calories + 31.5g protein
1 chicken breast (120g) = 198 calories + 37g protein
This lack of protein, paired with carbohydrate-rich eating habits is also a major driver of pathogenic infections, such as candida or yeast overgrowth, small intestinal bacterial overgrowth (SIBO), and can impair digestive function over time, increasing susceptibility for parasite and helicobacter pylori infections as well. I’ll explain more of this mechanism later in the post.
why i don’t work with clients who are unwilling to consume animal proteins
The short answer - their success and my reputation depend on it.
I have worked with clients in the past who prefer vegetarian and vegan diets, and the reality is - they do not celebrate the same successes that my omnivorous clients do when it comes to resolving their digestive symptoms, PCOS symptoms, and weight issues.
If that sounds too harsh, please know that I do hold space for different views on vegetarian vs vegan vs omnivorous diets, and can appreciate that there are many different reasons for choosing one over another.
This decision does not come from a place of judgment, but rather for the sake of the long-term health and success of the women who come to see me.
When it comes to symptoms of hormone imbalance, sleep issues, blood sugar management issues, weight loss, and irregular periods, a diet without animal proteins simply will not support their efforts to address symptoms.
Here’s where I see the biggest impacts.
HORMONE HEALTH
The women and female-bodied individuals who come to see me, often present with symptoms of hormone imbalance, be it a PCOS diagnosis, irregular periods, PMS symptoms, painful periods, mood and sleep disruptions around their periods, migraines around their periods, and weight gain in their belly or hips.
Aside from the obvious ovaries, hormones are largely modulated by the adrenal glands and the liver. The adrenal glands are responsible for producing any sex hormones that are not produced by the ovaries or testes, and the liver is charged with hormone balance, in that, it is responsible for deactivating and eliminating excess hormones to maintain balance.
A diet rich in carbohydrates, and especially low in protein, drives insulin resistance which disrupts the HPA (hypothalamus, pituitary, adrenal) axis and consequently, the ability of the ovaries and adrenal glands to produce hormones.
Additionally, when left unaddressed, this disruption leads to prolonged chronic stress, leading to adrenal fatigue, chronic inflammation, and abnormal thyroid labs. This is a highly complex topic that I go into more detail about here.
Finally, a liver that is overburdened with the job of constantly having to convert excess glucose into fat and glycogen may not be able to effectively metabolize and eliminate excess hormones well, exacerbating hormone imbalance symptoms.
BLOOD SUGAR BALANCE
If you wake up around 2:00 am most nights to pee, or get “hangry” between meals, you have blood sugar regulation issues. This, too, involves your liver and adrenal glands, and is highly driven by a carbohydrate-rich diet, among other things.
Additionally, carb and sugar cravings are common symptoms of the pathogenic infections we discussed earlier. You see, yeast and bacteria LOVE sugar, and when they infiltrate your gut, they live off of your resources. This perpetuates blood sugar imbalances, leading to insulin resistance, adrenal fatigue, and symptoms of hormone imbalance. (seeing a pattern here?)
GUT HEALTH
This topic is multifaceted, but here are the two main points I want to focus on for the sake of this post:
lack of protein inhibits digestion - Healthy digestion relies on many components - a regulated nervous system, optimal output of digestive juices (enzymes and stomach acid), and adequate chewing and mechanical digestion. Consuming protein tells your body to produce stomach acid (HCl) and proteolytic enzymes. With a low-protein diet, HCl production suffers, and so does your digestion. Since one of the main roles of HCl is to disinfect your food, poor HCl output leaves you more susceptible to pathogenic infections of the gut, driving inflammation, hormone issues, and overall discomfort.
migrating motor complex (MMC) - This important mechanism occurs only in a fasted state, and consists of a cascade of events intended to sweep out unwanted microbes from the small intestine. A carbohydrate-rich diet often makes one hungry more frequently throughout the day, leaving very little fasted time for the MMC to activate. If you are one who snacks or grazes throughout the day, you are doing your gut a disservice.
learn something new?
Please share your thoughts and questions in the comments below.
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
National Research Council (US) Subcommittee on the Tenth Edition of the Recommended Dietary Allowances. “Protein and Amino Acids.” Recommended Dietary Allowances: 10th Edition., U.S. National Library of Medicine, 1 Jan. 1989, www.ncbi.nlm.nih.gov/books/NBK234922/.
Hudson, Joshua L, et al. “Protein Intake Greater than the RDA Differentially Influences Whole-Body Lean Mass Responses to Purposeful Catabolic and Anabolic Stressors: A Systematic Review and Meta-Analysis.” Advances in Nutrition (Bethesda, Md.), U.S. National Library of Medicine, 1 May 2020, pmc.ncbi.nlm.nih.gov/articles/PMC7231581/.
Association of Major Dietary Protein Sources with All‐cause and Cause‐specific Mortality: Prospective Cohort Study | Journal of the American Heart Association, www.ahajournals.org/doi/10.1161/JAHA.119.015553. Accessed 3 Oct. 2025.
The Role of Protein in Insulin Resistance Symptoms and Treatment
And still, you've bought into vegan protein shakes, and have shelves loaded with protein-enriched cookies, bars, and cereals. You’re feeling pretty good about meeting those higher protein intake recommendations that saturate your social feed.
But I’m here to dig deeper into the role of protein in insulin resistance symptoms, and why getting your protein from those sources might be making your insulin resistance symptoms worse, contributing to weight gain and inflammation.
The role of protein in insulin resistance treatment
If you’ve followed me for any amount of time, you know that what’s missing from those posts from fitness influencers you follow on TikTok, is nuance. That’s what I bring to the table.
You might have already read my articles about protein quality and the health effects of a vegan diet. And still, you've bought into vegan protein shakes, and have shelves loaded with protein-enriched cookies, bars, and cereals. You’re feeling pretty good about meeting those higher protein intake recommendations that saturate your social feed.
But I’m here to dig deeper into the role of protein in insulin resistance symptoms, and why getting your protein from those sources might be making your insulin resistance symptoms worse, contributing to weight gain and inflammation.
Hi darlings. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress, insulin resistance, and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between their lab values and what their body is saying. Before you continue, click here to read my Medical Disclaimer.
In this article, you’ll learn:
what is insulin resistance?
insulin resistance causes and symptoms
the role of protein in insulin resistance treatment
why protein quality matters just as much as quantity
more ways to improve insulin sensitivity symptoms
what is insulin resistance?
The word metabolism often gets referred to as one’s ability or inability to lose weight. But the word metabolism actually refers to the conversion of one component into another.
With digestion, metabolism might refer to ingested food being broken down into nutrients your body can use. Or a chemical component of medication or a food additive might be manipulated by enzymes into a neutralized form and removed from the body.
For the sake of this discussion, we’ll be referring to metabolism in regard to glucose metabolism - the conversion of glucose (a molecular form of sugar) into energy or fat.
It’s important to understand that glucose comes from more than just sugar ingredients. Glucose comes from all carbohydrates, including grains, starches, and yes, sugar.
So, whether it’s potatoes, sweet potatoes, rice, bread, legumes, fruit, honey, or candy - it all turns into glucose.
And that glucose either gets metabolized into energy or fat. Insulin, a hormone produced by the pancreas, is required for the metabolism of glucose into energy.
Here’s how glucose metabolism works:
When you consume any kind of carbohydrate, be it starchy legumes, grains, or vegetables, sugars like honey, fruit, or cane sugar, even leafy greens contain carbohydrates - those carbohydrates are broken down into molecules called glucose.
Glucose molecules are transported into your bloodstream through the epithelial lining of the small intestine. The amount of glucose molecules in your bloodstream at any given time is referred to as your “blood sugar” or “blood glucose” level.
Insulin is released by the pancreas and acts as sort of an usher, taking the glucose to individual cells, and using its key to unlock the door (insulin receptors embedded in the cell membrane) and shuttles the glucose in to be metabolized (hey, there’s that word again!) via the Krebs cycle within the mitochondria.
When cells have had their fill of glucose, any glucose remaining is then sent to the liver and converted to storable forms of glucose, specifically glycogen and triglycerides.
Glycogen: stored primarily in the liver, and to some extent, muscles. The liver has a very small capacity for glycogen storage.
Triglycerides: stored as fat tissue, also called adipose tissue. Your body has unlimited stores of triglycerides in adipose tissue, as it can always (and does) make more fat to accommodate more triglyceride storage.
HERE’S WHERE THINGS CAN GO WRONG
Insulin resistance occurs when there is regularly more glucose than can be used by cells in the bloodstream. For example, one who consumes a high-carbohydrate diet at most meals and snacks will likely develop insulin resistance symptoms.
When there is regularly more glucose in the bloodstream than cells can accommodate, insulin receptors (remember the locked doors on cell membranes) begin to deactivate, making insulin ineffective. The cells are essentially saying, “we’ve had enough!”.
In response, the body produces more insulin to try and compensate for glucose not getting into cells, and as a result, insulin resistance worsens.
And what happens to glucose that does not enter cells? It gets converted to fat.
insulin resistance causes and symptoms
COMMON CAUSES OF INSULIN RESISTANCE
high starch, high carbohydrate diet
regular consumption of processed foods (including foods you might consider “health foods”, like protein powders, bars, shakes, and plant-based meat substitutes)
chronic stress (external or internal) - Click here to read more about the role of cortisol in blood sugar regulation
inactivity/sedentarianism
inadequate sleep
overexercising (especially cardio)
pancreatic insufficiency (more on what symptoms look like later in the article)
leaky gut syndrome
COMMON SYMPTOMS OF INSULIN RESISTANCE
weight gain in belly and/or hips
difficulty losing weight
“hangry” symptoms between meals (loss of focus, shaky, irritability)
digestive symptoms
pancreatic insufficiency can often contribute to digestive dysfunction, as it is needed to produce digestive enzymes
digestive symptoms are often indicative of pathogenic infection, such as yeast or bacterial overgrowth, mold, or parasites - all of which contribute to chronic stress response and cortisol output
excess hunger (frequent hunger, or excess appetite)
Type II Diabetes diagnosis, or pre-diabetes
abnormal thyroid labs (click here to read more)
sweet, salty, or carb cravings
the role of protein in insulin resistance treatment
It’s no secret that we need protein to build muscle - and that’s exactly the same reason it’s needed for insulin resistance treatment.
Let me explain.
HOW YOUR BODY BUILDS MUSCLES
A common misconception about building muscles, is that it requires an increase in the number of muscle cells (also called muscle fibers) - but this is incorrect. Your body actually cannot produce more muscle cells.
Muscle cells can, however, get larger in size - this is what is known as hypertrophy.
Additionally, contained in the fluid between muscle cells are smaller stem cells called satellite cells. In addition to hypertrophy, the satellite cells are the catalyst between protein and muscle development.
When you exercise, especially through resistance training, small tears develop in your muscle fibers. Your body responds to these tears by branching together amino acids (the building blocks of protein) together with satellite cells, to repair the tears and make the muscle stronger.
This process requires both adequate dietary protein and resistance training.
What does that have to do with insulin resistance treatment?
Earlier we talked about how glucose is converted to ATP in the mitochondria of the cells. You might remember from middle school science class that the mitochondria are known as the “power house” of the cell.
Here’s where it connects to insulin resistance treatment >>> Resistance training stimulates mitochondrial biogenesis - meaning the creation of more mitochondria - within muscle cells. This is due to the increased need for energy when building and using muscles.
Thus… increased mitochondria = increased need for glucose to create energy = increased glucose uptake into muscle cells.
In fact, it’s important to remember that the research has been clear for years, that as we age, muscle tissue degrades, a condition called sarcopenia. Resistance training has been shown to prevent sarcopenia and improve insulin resistance [1].
all proteins are not created equal
There’s a lot of push from wellness influencers for more women to eat more protein - and they are not wrong (as you can see from our previous discussion).
Protein is needed for nutrient transfer into cells, for neurotransmitter synthesis (mood and sleep regulation), muscle building, and many more reactive and enzymatic processes throughout the body.
What those influencers are not telling you is that the quality of protein matters. Big time.
Having a shelf stocked with protein powders, bars, shakes, and cereals all touting that they are “protein-packed”, you might be missing the mark - especially if those products are made with plant-based proteins.
A FEW THINGS YOU MAY NOT KNOW ABOUT PROTEIN:
plant-based proteins cannot be absorbed and utilized in the body as efficiently as animal proteins [2]
eating more protein can increase health concerns if you have digestive symptoms
in addition to reduced bioavailability, you cannot meet optimal protein intake goals from plant-based sources without also consuming loads of starchy carbohydrates and extra calories - this works against your efforts to resolve insulin resistance symptoms
there are nine amino acids that the human body requires, but cannot make for itself - these are called essential amino acids
it’s important to consume a wide variety of proteins (as well as other foods) to ensure you are getting all essential nutrients required by the body. Additionally, eating the same foods every day is a great way to develop food sensitivities.
EXAMPLE: You would have to consume 700 grams of boiled chickpeas, which contain all nine essential amino acids, to meet your protein intake goals for one day. That’s also 1200 calories, and over 140 grams of starchy carbohydrates. Quinoa and soybeans have similar profiles - imagine eating 6 cups of quinoa to meet your protein intake goals!
MY TAKE ON THE ENVIRONMENTAL IMPACTS OF ANIMAL PROTEINS
TL;DR
Opting out of meat and consuming only plants is not the answer to addressing environmental distress, and especially not your physical health. If your resources allow, consider supporting the farmers who are doing the work to improve environmental impact, so that down the road, this will be more accessible to everyone.
THE DIRT
I greatly value the health of our environment, and do everything within my power to make it better for the next generation. Because of that, I have done a lot of research on the impacts of farming, both livestock and plants, on the environment, and a few things have become very clear:
regenerative farming techniques are showing robust evidence that they actually improve soil quality and sequester carbon - we need to change the way we farm animals, not do away with them altogether. You can help by actively supporting the farmers who are doing this work.
the information being presented in documentaries like [unnamed] has been wildly misrepresented - I urge you to look at the research for yourself.
the amount of waste that comes from processed foods like cereals and plant-based meats is astounding and has a significant impact on environmental health just as much as conventional animal farming. Subsidized grain farms have tilled the soil to the point of desertification, and it needs to stop. Cutting out meat is not the answer.
more ways to improve insulin resistance symptoms
Building muscle is not the only way to combat the effects of insulin resistance. Improving insulin sensitivity is not difficult, but it requires consistency. Here are a few ideas to get you started:
STOP SNACKING
The good news is, increasing protein intake with each meal will help keep you fuller for longer periods of time. When my clients add more protein to their diets, they effectively stop snacking, too. This will help steady your blood glucose levels throughout the day, rather than continuously creating glucose spikes that perpetuate insulin resistance symptoms.
ALTERNATE DAY FASTING
The effects of alternate-day fasting on improving insulin sensitivity are astounding. Not only does fasting increase growth factors that help you build muscle, but when done properly, it increases the sensitivity of your insulin receptors, and helps your body to adapt to using fat for fuel when glucose is not available. It’s extremely important to note that refeeding after fasting is an important part of the process, and learning to fast for health effects is essential. Click here to learn how to fast safely and healthfully.
IMPROVE YOUR MACRONUTRIENT BALANCE
If you’re getting all your protein from a shake stuffed with pea protein isolates, you are doing your body a disservice. Use this guide to build healthier meals that give your body everything it needs to keep you fueled.
FIND AND ADDRESS UNDERLYING CAUSES OF STRESS
Chronic stress, whether from work, relationships, lack of boundaries, or underlying dysfunction in the body, drives insulin resistance and inflammation. Finding and addressing underlying causes of stress, such as digestive dysfunction, adrenal fatigue, or pathogenic infection from yeast overgrowth, parasites, or bacteria, can be pivotal to your insulin resistance treatment. Here’s how I can help.
learn something new?
Please share your thoughts and questions in the comments below.
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
The Heart of Physiological Reports - Lindsey - 2024 - Physiological Reports - Wiley Online Library, physoc.onlinelibrary.wiley.com/doi/10.14814/phy2.15962. Accessed 3 Oct. 2025.
Association of Major Dietary Protein Sources with All‐cause and Cause‐specific Mortality: Prospective Cohort Study | Journal of the American Heart Association, www.ahajournals.org/doi/10.1161/JAHA.119.015553. Accessed 3 Oct. 2025.
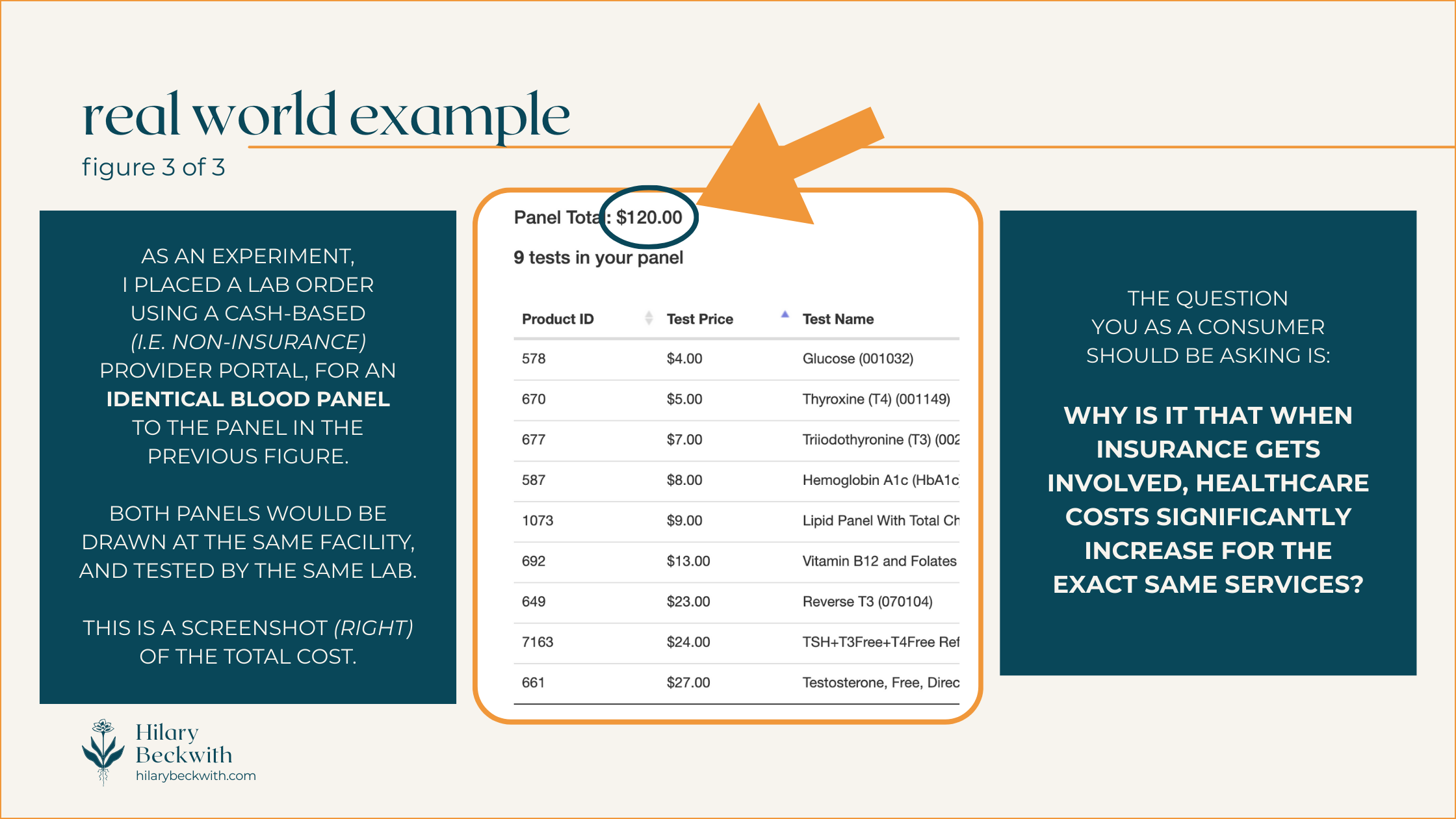
Why Your Health Insurance Plan Won’t Cover Functional Nutrition
One thing is common for us all - we are wildly in the dark about how health insurance works and who decides what’s covered. That is why my intention with this article is to offer clarity and education, so you can stop blindly allowing your health insurance plan choose your providers for you, and make more informed health decisions for yourself.
Why Your Health Insurance Plan Won’t Cover Functional Nutrition
It’s no secret that the healthcare system in the U.S. is a bumbling sh*tshow. We’ve privatized health insurance plans since the 1920s, causing costs to soar, excluding important health services, and making plans effectively useless to those who are relatively healthy.
It’s a complex issue, and a highly controversial one. I’ve worked in healthcare for 20+ years, both on the clinical side, and the billing side. I can’t change our severely broken system on my own. But, one reader at a time, I can help individuals like you know how to advocate for your own health when seeking out health insurance plans and healthcare services.
Hi darlings. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between what their doctor is saying and what their body is saying. Click here to read my Medical Disclaimer.
In this article, you’ll learn:
is health insurance necessary?
what it means to use an “in-network” provider
the difference between “covered” and “non-covered” services (it might not be what you think)
is health insurance necessary?
For about nine years in the early 2000s, I worked for a large chain grocery store. I wore many hats there, but one of my jobs was to help change price tags when a new ad started every Wednesday.
I and my crew would replace expired sales tags with their regular price, as well as replace regular-priced tags with the new sales tags.
Every sales tag also showed the product’s regular price, so you as the customer could see how much you were saving by getting it on sale.
Here’s where things get shady…
Very often, when a product would go on sale, the store would increase the regular price of that item so that it looked like you were saving more money. When the sale ended, the regular price went back to its normal market rate.
In other words, the regular price on a sale item was completely arbitrary - it was used as a marketing tool to show how much the customer would “save”. [insert barfing noise]
Here’s the thing… Your health insurance plan does the same thing.
I’ll talk more about that later in the post. But first, let’s explore whether a health insurance plan is even necessary to have.
holding space
I want to be clear - the realities that we all live in are so different. What I have to say in this article will not relate to everyone. We each have different values and different needs to consider when choosing healthcare services and utilizing health insurance plan benefits.
One thing is common for us all - we are wildly in the dark about how health insurance works and who decides what’s covered. That is why my intention with this article is to offer clarity and education, so you can stop blindly allowing your health insurance plan choose your providers for you, and make more informed health decisions for yourself.
It is not at all meant to suggest that no one benefits from using health insurance. Plenty of individuals rely on private, state, and federally funded insurance plans to provide treatment for chronic illness and other medical conditions, and I hope to present this article with some sensitivity to that.
Earlier this summer I had a pretty serious injury - I fell while rollerskating, fracturing my ankle in three places, dislocating the joint, and detaching a ligament.
It required a trip to the E.R., surgery to repair the damage, multiple sets of imaging (before and after surgery), physical therapy, etc..
As a functional nutrition practitioner, I often look to treatment options that are root-cause-focused, as opposed to symptoms-focused. An injury like this requires a different approach.
I leaned into Western medicine (mostly covered by my health insurance plan), but I also utilized my nutrition background to optimize my healing, support bone density, regulate inflammation, regulate my nervous system after a traumatic injury, and support detoxification from pain meds (all not covered by my insurance).
So, was it necessary to have a health insurance plan in this instance?
I would argue yes… sort of…
I’ve already put in thousands of dollars toward premiums over the four years I’ve had this health insurance plan. Was it worth it for peace of mind? That’s debatable. Many Americans are terrified that the cost of healthcare, even with insurance, will lead them to crippling debt. You can read about my research on this topic here.
I certainly think there is a place for insurance, and an accident like this one is a good example of when insurance is necessary. But privatized insurance has been driving healthcare costs up (and up, and up…) since the 1920s [1], making quality healthcare largely inaccessible to many in the low or middle classes nearly 100 years later.
We’re all stuck between a rock and a hard place.
using an in-network provider
I think most of us understand that when using health insurance plan benefits, the question we most commonly ask a practitioner is, “do you take my insurance?”. After all, being in-network means the care will be cheaper, and in some cases is the difference between coverage or no coverage.
After working for nearly 25 years in medical clinics, I’ve learned that most people do not understand how their insurance works. And who can blame you!
SOME THINGS YOU MAY NOT KNOW ABOUT HEALTH INSURANCE:
INSURANCE IS A CONTRACT
The patient has a contract with their health insurance plan, as do any in-network practitioners. As with any contract, the terms look different for every health plan, but in general, the terms of patient-insurance contracts boil down to this:
IF the patient pays their portion, THEN insurance will pay theirs. Despite common belief, it is not the other way around.
PRACTITIONERS ARE NOT REQUIRED TO SUBMIT CLAIMS
It is not the responsibility of a practitioner to submit claims or pre-authorization requests on behalf of a patient. Practitioners typically take it on themselves simply because it’s easier for them to directly supply the information required by the insurance company, rather than have the patient be a liaison.
IT IS THE PATIENT’S RESPONSIBILITY TO UNDERSTAND THEIR OWN BENEFITS
Some practitioners are kind enough to give patients a cost estimate for care based on their insurance benefits - but it is not the practitioner’s responsibility to do so.
IT IS THE PATIENT’S RESPONSIBILITY TO APPEAL
Very often, health insurance plans deny services that should be covered according to the plan benefits (I recently experienced this, myself). In many of those cases, the practitioner is kind enough to submit an appeal on the patient’s behalf, again, because it is easier for the practitioner to directly submit required documentation. But it is not the practitioner’s responsibility to do so.
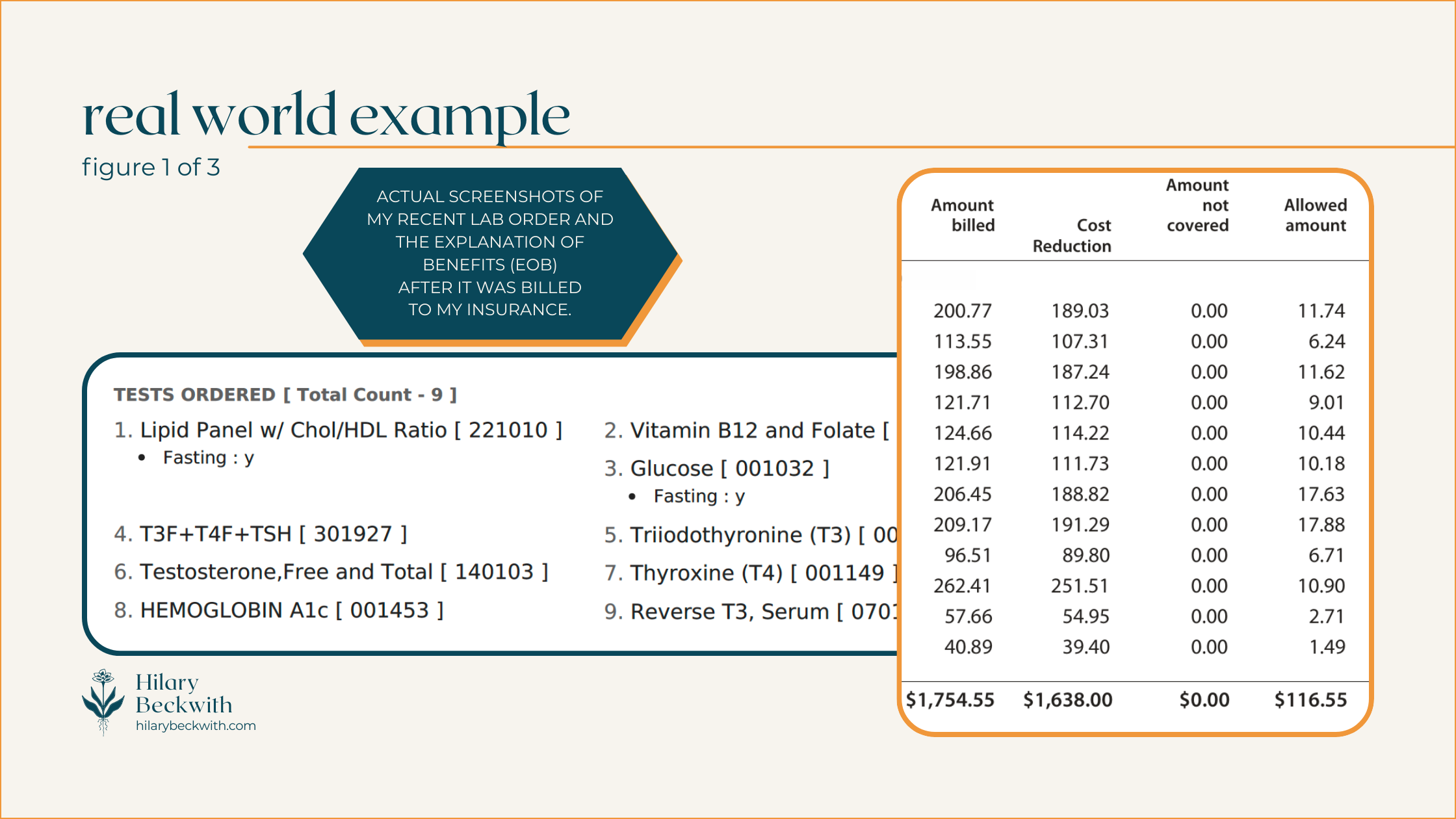
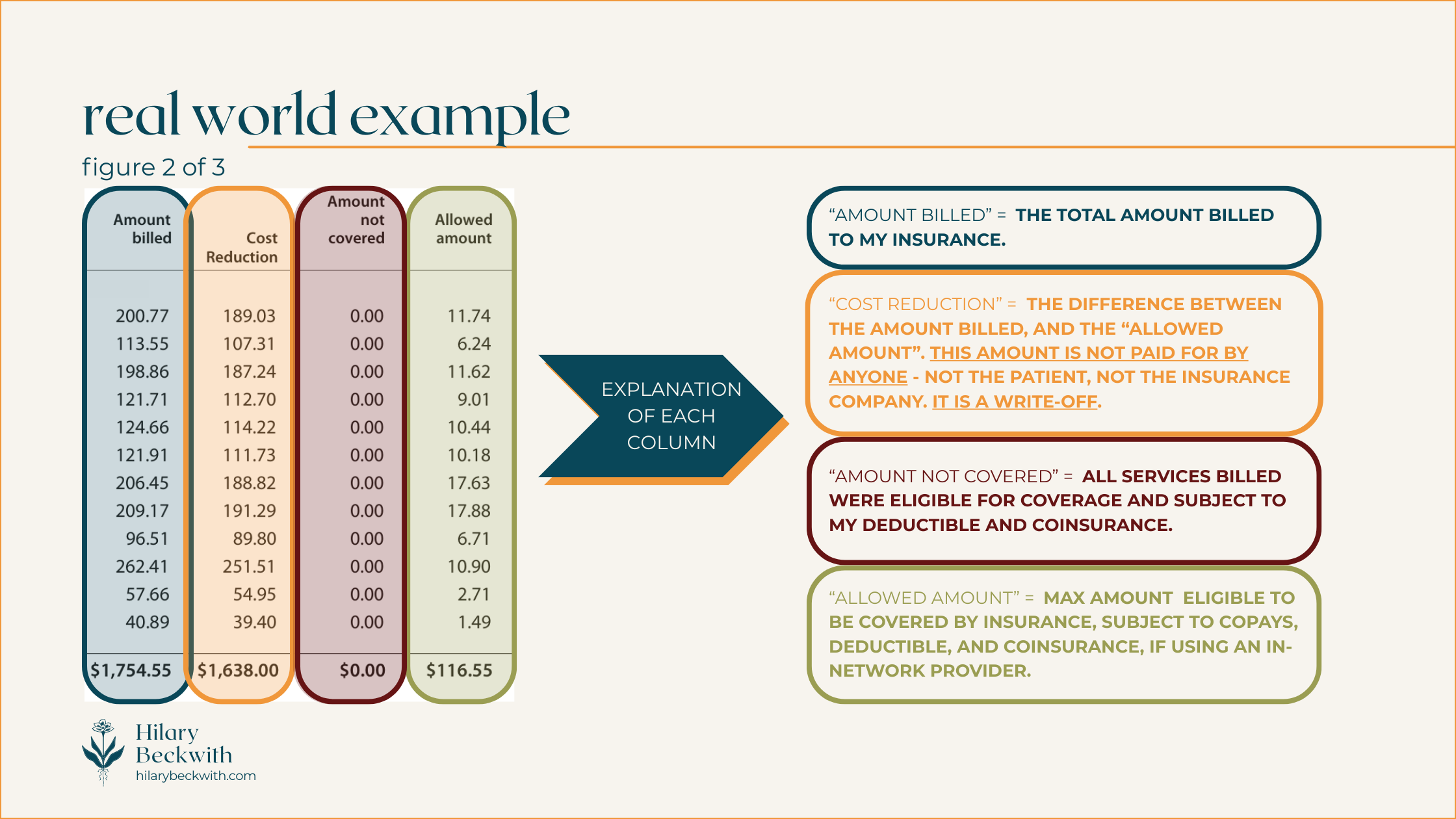
A PRACTITIONER WHO IS IN-NETWORK, TAKES A PAY CUT
If a practitioner is in-network with your health insurance plan, it means they have a provider-insurance contract with the insurance provider. That contract, in essence, says that in exchange for advertising (i.e. a directory, or network, of “preferred” practitioners), practitioners agree to discount their care, so that the insurance does not have to pay out as much.
Patients will often see these discounts conveyed as “you saved $___!” on their Explanation of Benefits (EOB).
IN-NETWORK PRACTITIONERS MAY BE LESS LIKELY TO SEEK OUT ROOT CAUSES OF YOUR SYMPTOMS
When practitioners are contracted with an insurance plan, they are subject to the regulations of that plan.
A common example of this is regarding thyroid testing. Many health insurance plans in the U.S. stipulate that in order to diagnose hypothyroid, TSH must be high, and free T4 must be low. Therefore, even if the patient has many other indications of hypothyroidism, your in-network practitioner will likely only test for TSH and fT4, unless you request otherwise.
Put more simply, health insurance plans are not designed to keep relatively healthy people, healthy. Health insurance plans are designed for symptoms-focused care and injuries.
Most health insurance plans do not cover services designed to optimize your health, such as functional lab testing, somatic work, treatments for complex trauma, and, yes, holistic nutrition consulting.
They’ll happily cover sleep medications, blood pressure medications, or weight loss surgery - but they will not cover the types of care needed to address root causes of insomnia, high blood pressure, and weight gain.
covered v. non-covered services
Health insurance is confusing - that’s why I’m here to bring some clarity to your world when navigating healthcare decisions, and those confusing EOBs.
I’ve included some diagrams below to help you understand things a bit better. But first, let’s talk vocabulary.
WHAT DO THESE COMMON HEALTH INSURANCE TERMS MEAN?
COVERED SERVICES:
A “covered” service is any service that is eligible for coverage, meaning it meets criteria set by the health insurance plan, including diagnosis, practitioner type, and plan inclusions.
A service that’s “covered” does not necessarily mean it is paid for by your insurance. A “covered” service is still subject to your plan benefits, such as deductible, coinsurance, or co-pay.
NON-COVERED SERVICES:
A “non-covered” service is any service that does not meet criteria set by the health insurance plan. The cost of a non-covered service is entirely the responsibility of the patient.
A service might be considered “non-covered” for the following reasons:
it is specifically excluded from your health insurance plan benefits
it was provided by an excluded practitioner type (e.g. a blood draw may not be covered if it is performed by a Naturopath if Naturopaths are excluded from your plan)
your diagnosis does not meet the requirements set by your insurance plan for the service to be covered - this does not mean your practitioner incorrectly diagnosed you.
the service was performed in a non-covered clinic or facility (e.g. getting Physical Therapy in a hospital setting may be covered differently than it would in an office setting).
IN NETWORK
Indicates a practitioner, facility, or group of practitioners, are contracted with a health insurance plan. As we discussed earlier, services from an in-network practitioner usually indicates “covered” service costs will be discounted.
OUT OF NETWORK
Indicates a practitioner, facility, or group of practitioners, are not contracted with a health insurance plan. Out-of-Network does not necessarily mean services will not be covered - but it does mean the costs will not be discounted.
DEDUCTIBLE
A dollar amount set by your health insurance plan, if applicable, that the patient must pay before the insurance begins paying for services. Coverage after the deductible is met varies from plan to plan.
EXAMPLE: If your insurance has a $1000 deductible, you must pay for services in full until they reach a total of $1000, after which your insurance will start paying according to your plan benefits. This only applies to “covered” services. Any non-covered services will not apply toward your deductible.
COINSURANCE
Not to be confused with a co-pay, a coinsurance is a percentage set by a health insurance plan that the patient is responsible to pay for all covered services. Most often, a plan that includes a coinsurance also includes a deductible, and similarly only applies to “covered” services.
EXAMPLE: If your insurance requires you to pay a 20% coinsurance, your insurance would pay 80% of covered services, and you would pay 20%. Typically this is applied after a deductible has been met.
CO-PAY
A co-pay is a flat-rate amount set by a health insurance plan that patient is responsible to pay for every eligible practitioner visit. Co-pay plans are very rare these days, and typically do not entail a deductible or coinsurance.
EXAMPLE: If your health insurance has a $30 co-pay, you would pay $30 when visiting a covered practitioner providing covered services, and insurance would pay for the rest. Some insurance plans may require separate co-pays for different types of services, even if they are provided by the same practitioner in the same day (e.g. a physical exam and a spinal manipulation may require two separate co-pays for the same visit)
do I take insurance?
Nope!
Or rather, it’s that insurance doesn’t take me.
As you’ve learned in this post, health insurance plans in the U.S. are more likely to cover treatments designed to suppress symptoms or change lab values.
It might even help you feel better for a time. But it won’t be the solution to your PCOS symptoms, IBS symptoms, weight gain, or anxiety. Those symptoms will all still be there the moment you stop taking the medications.
That’s why my work is focused on helping clients find and address root causes of their symptoms, not just changing lab values.
want to see what you’re missing?
learn something new?
Please share your thoughts and questions below.
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
Friedman, Jordan. “How Health Insurance Got Its Start in America.” History.Com, A&E Television Networks, 27 May 2025, www.history.com/articles/health-insurance-baylor-plan.
Inflammation Foods - Anti Inflammatory Diet Nutritionist
Your body uses inflammation to fight off everything from infection, to allergies, to tissue injury.
But when any of those things goes undiagnosed or untreated, inflammation becomes chronic, exacerbating pain levels and other symptoms. And the foods you eat can either help or hurt your healing potential.
Inflammation Foods to Avoid
Inflammation hits in so many ways, but easily the most obvious manifestation of inflammation is pain. Whatever the cause of your pain symptoms, it’s important to recognize pain as your body’s alarm system. Your body uses inflammation to fight off everything from infection, to allergies, to tissue injury.
But when any of those things goes undiagnosed or untreated, inflammation becomes chronic, exacerbating pain levels and other symptoms. And the foods you eat can either help or hurt your healing potential.
Hi friends. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between what their doctor is saying and what their body is saying. Click here to read my Medical Disclaimer.
In this article, you’ll learn:
signs of inflammation
causes of systemic inflammation
when to seek help
foods that reduce inflammation
signs of inflammation
Ironically, and perhaps inspirationally, I am writing this blog from my bed as I keep my recently fractured ankle elevated. Needless to say, it got me thinking about the process of pain and healing. And since I love working with clients who have inflammatory conditions, I thought this a great time to share some tools that might help you.
To start, pain is not the only sign of inflammation, just as nutrition is not the only solution for it. Let’s talk about what defines inflammation.
An inflammatory response is when your body sends white blood cells (from the immune system) to a specific area, or systemically, in order to heal tissue or fight off foreign invaders like viruses, parasites, dysbiotic bacteria, or mold toxins.
Probably the easiest way to visualize inflammation that most of us can relate to is a cold or sinus infection. That snot you’re blowing out and that stuffs you up and keeps you from breathing? This is acute inflammation.
That’s your mucous membranes being activated due to an immune system response to an unwanted pathogen. And as miserable as you might feel in those times, it’s your body is doing what it’s supposed to.
However, when you have chronic sinus infections, seasonal allergies, or chronic “stuffy head” - this is chronic inflammation.
Inflammation plays an important role in healing and helping us to survive as a species. But what’s missing is the regulation of inflammation. Our modern lifestyle of processed foods, unaddressed complex trauma, and excess busyness, fosters chronic inflammation. And unfortunately our American healthcare system does very little to address root causes of inflammation, focusing only on treating the symptoms.
Keep reading so you can be better informed and advocate for your health at your next doctor’s visit.
SIGNS OF INFLAMMATION (acute or chronic):
pain
localized swelling
acne
eczema
sinus congestion
seasonal allergies or food allergies
fatigue
restless sleep or insomnia
digestive symptoms (bloat, diarrhea, indigestion, abdominal pain)
brain fog
excess appetite
craving carbs or sweets
female reproductive hormone imbalance (irregular periods, infertility, painful periods, etc.)
causes of chronic inflammation
When the causes of acute inflammation go unaddressed, we get chronic inflammation.
The body is still trying to fight, but is running out of resources, so it tends to trickle in support, rather than offer a full-fledged army. Over time, your body does what it can to preserve energy, and so it activates the Cell Danger Response [1].
During Cell Danger Response, or CDR, your cell walls stiffen in an effort to prevent nutrients from entering the cell for energy production, they send out hormone signals to summon your immune system for additional support, and an enzyme called deiodinase 3 is activated, which deactivates thyroid hormone, converting it to its opposite, reverse T3. Click here to read more about thyroid conditions.
This chronic inflammatory response is commonly referred to as low-grade inflammation, or systemic inflammation. While it may have started in a specific area of the body, left unaddressed, it can become a low-grade inflammation throughout the body.
This is where we begin to see conditions like:
pain that will not go away
autoimmune disease activation
abnormal thyroid levels being misdiagnosed as a thyroid issue
treatment for symptoms without addressing underlying cause (acne, digestive symptoms, allergies)
chronic fatigue
COMMON CAUSES OF SYSTEMIC INFLAMMATION
So, what is behind all these symptoms? It’s true that chronic pain can come from a tissue injury that didn’t heal properly, excess scar tissue, nerve damage, or possibly more overlooked, your nervous system trying to protect you even after the tissue has healed.
In many cases, the chronic inflammation requires a multifaceted approach:
physical medicine (PT, chiropractic, massage, trigger point injections, Platelet-Rich-Plasma, etc.) to heal the injured tissue
nutritional support to reduce inflammatory foods
functional support to find and address root causes of inflammation that have previously gone unnoticed
mental health support for nervous system regulation. Chronic cortisol production from a constant, or nearly constant, state of fight or flight activation (excess busyness, poor sleep, anxiety, depression, etc.) increases inflammation.
Although much of my career was spent working in physical medicine, I cannot expertly speak to the physical tissue healing or mental health aspects of inflammation. You can find support for those aspects here:
But I can speak to functional and nutritional causes of inflammation. Addressing these types of inflammation requires more strategy than simply avoiding high inflammation foods, or following an anti inflammatory diet.
Let’s talk about nutritional and functional causes of inflammation before we get into the possible solutions.
nutritional and functional causes of inflammation
There can be many causes of systemic inflammation that contribute to chronic pain, skin conditions like acne or eczema, digestive symptoms, chronic fatigue, or seasonal allergies.
This list is certainly not exhaustive, but these are common issues I find in many of my clients. And when we work to address these underlying issues, we often find that their symptoms reduce or dissipate altogether.
COMMON NON-INJURY CAUSES OF SYSTEMIC INFLAMMATION:
pathogenic infection - I commonly find underlying infections that have previously gone unnoticed, undiagnosed, and thus, untreated, in my clients. Pathogens like parasites, mold, mold toxins, candida overgrowth, or dysbiotic bacteria. Left unchecked, these infections cause a constant stimulation of the immune system, and consequently, systemic inflammation.
food sensitivities - The ultimate chicken-and-egg scenario, food sensitivities are an immune response to foods that have not been properly broken down by the digestive system, and thus make it into the bloodstream, only to be responded to as a foreign invader - a threat. Food sensitivities are not to be confused with food allergies, and symptoms can often look like increased congestion, runny nose, achyness, stiffness, or increased pain, or reactive digestive symptoms like diarrhea.
poor digestive health - Sound too simple? Your digestive system is the first line of defense against pathogens that are ingested through foods. Poor digestion is one of the first things I address in clients with chronic inflammation for this very reason. Your body needs adequate stomach acid and digestive enzymes, a healthy mucosal lining, and good motility to prevent pathogens from getting into your system and to eliminate toxins. The overuse of antacids, eating on-the-go, and excess busyness inhibit your body’s ability to eliminate pathogens before they become a problem. Additionally, poor digestion is a common cause of food sensitivities. Addressing and optimizing digestive health is fundamental to reducing systemic inflammation.
poor quality diet - as we discussed, it’s not so much about following an anti inflammatory diet, but more about the quality of nutrition, and addressing gut health. If you are eating poor-quality foods, your body is getting poor-quality nutrients and overloading your liver.
A good example of this is fats:
Fats are broken down into fatty acids which are needed throughout the body for cell membrane structure, hormone production, vitamin D formation, bile production, and, yes, inflammation regulation. If you are eating poor quality fats, and if your body is not digesting fats well, of course your body is inflamed!
Fats are not the only culprit:
Refined grains, excess starches and sugars from plant-based meats and dairy products, food additives, emulsifiers, gums, even the cookware you choose, all contributes to inflammation by increasing toxic burden and oxidative stress. Learn more about how to choose quality foods here.
when to seek help
Addressing chronic inflammation requires more than just avoiding high inflammation foods, or following an anti inflammatory diet.
Yes, there are foods that can help lower inflammation, however, if you have sensitivities to those foods, or are not digesting them well, an anti inflammatory diet will not help you for very long.
You may notice some improvement initially, but it will likely be short-lived until you address underlying causes.
If you are already actively working with practitioners to address tissue injury, structure, nerve dysfunction, and your pain still persists, it’s possible there is an underlying cause that has gone unnoticed or unaddressed.
If you experience even a few of the symptoms below on a regular basis, it’s time to dig deeper into the root causes.
SIGNS OF SYSTEMIC INFLAMMATION:
known food sensitivities or food allergies
suspected food sensitivities (you have noticed a pattern of symptoms within 24 hours of consuming specific foods). Click here to read more about symptoms of food sensitivities.
acne
eczema
chronic diarrhea or constipation (or alternating)
bloating after meals
excess hunger
craving carbs or sweets
pain that has been difficult to address, despite physical medicine efforts
chronic stuffy head or runny nose
seasonal allergies (while there may be an actual allergic reaction, seasonal allergies can also be an overreaction of the immune system due to overburden, and can be alleviated with proper support)
chronic fatigue
anxiety or other mood conditions
insomnia or other sleep issues
chronic heartburn or indigestion
abdominal pain or cramping
Working with a qualified practitioner to find and address root causes of inflammation can help alleviate chronic pain symptoms and may even reduce your need for pain medications.
foods that reduce inflammation
As I’ve pointed out, reducing systemic and chronic inflammation requires more than simply eating an anti inflammatory diet or avoiding high inflammation foods.
It requires intervention from a qualified practitioner trained to find and address root causes of dysfunction and gut health in your body. This process often requires a proper assessment of the individual, including symptoms, health history, food and lifestyle habits, and functional lab testing.
Following an anti inflammatory diet may not be the solution, but it certainly can help if it’s part of the equation!
Here are some tips for lowering inflammation using nutrition:
eat real food: Even foods that are marketed as being “healthy” can be heavily processed, and a burden on your detoxification system. Not sure what makes food “processed”? Click here to learn more about what to look for on the ingredients list.
pay attention to fats: Put briefly, omega 3 fatty acids are anti-inflammatory, and omega 6 fatty acids are pro-inflammatory. The most bio-available (can actually be used by the body without interference) and nutrient-dense sources of omega 3 fatty acids are found in animal sources, such as grass-fed beef and wild caught salmon.
fish oil supplements: As with food, when it comes to supplements, quality matters. There are many fish oil supplements on the market, and most are garbage. They use irresponsible fishing methods, and use ethyl (alcohol) ethers of the fatty acids, which are far less absorbable than triglycerides. But there is one fish oil supplement I love and recommend often that is ethically sourced and highly bioavailable. Click here to view and purchase.
eat brightly-colored whole foods: Brightly-colored vegetables, such as in-season tomatoes, red, orange, and yellow bell peppers, and purple cabbage, are loaded with antioxidants, such as bioflavonoids and polyphenols. While it’s important to find and address the root causes of oxidative stress (free radical damage), consuming lots of antioxidants can help mitigate the damage and lower inflammation.
eat better protein: While every body’s needs are different, my clients who are navigating inflammation, hormone imbalance, and digestive issues, get better results when they focus on getting enough good quality protein.
Getting adequate bio-available protein each meal helps reduce snacking, supports mood regulation, and reduces reliance on carby snacks, which lowers inflammation. Animal sources of protein are far more bio-available than plant-based (click here to learn more about that). Personally, I aim for 30 grams of protein in every meal, mostly animal-based.
hydrate: Yes, really! Good hydration promotes healthy lymphatic flow, which serves, in part, to transport components of your immune system and carry debris and waste to elimination sites. Hydration can also lower blood pressure and is important for liver function.
How much water should you drink? It varies from person to person. For the average active adult with no kidney problems, I typically recommend half your body weight, in fluid ounces of water, every day. It’s also important to minimize dehydrating factors, such as alcohol or caffeine. If you are someone who deals with chronic diarrhea symptoms, this may also be dehydrating you.
other supplements to lower inflammation: Taking supplements is a waste of your resources if you are not also doing the work to address the root cause. But symptomatically, there are some supplements that can help lower inflammation and help reduce pain symptoms. Here are some of my favorites.
boswelia - from the bark of a boswelia tree, this extract is a powerful anti-inflammatory agent.
pycnogenol - another park extract, from the French Maritime Pine tree, this nutrient is loaded with polyphenols and bioflavonoids to combat oxidative damage and reduce inflammation.
Oxicell-SE (Apex Energetics) - one of my favorite topical products from working in pain management, this product supports mitochondrial function at the site of pain, which helps to heal tissue faster and reduce inflammation.
curcumin - Curcumin is the active anti-inflammatory component of turmeric. It is widely known to be very effective at reducing inflammation [4], and because it is fat-soluble, it’s absorption significantly increases when taken with healthy fats [5].
was this helpful?
What has helped you address root causes of pain and inflammation?
Please share your thoughts and questions below!
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
Naviaux, Robert K. “Metabolic Features of the Cell Danger Response.” Mitochondrion, Elsevier, 24 Aug. 2013, www.sciencedirect.com/science/article/pii/S1567724913002390.
Astrup, Arne, et al. “Dietary Saturated Fats and Health: Are the U.S. Guidelines Evidence-Based?” Nutrients, U.S. National Library of Medicine, 22 Sept. 2021, pmc.ncbi.nlm.nih.gov/articles/PMC8541481/.
Di Grigoli, Antonino, et al. “Effects of Grazing on the Behaviour, Oxidative and Immune Status, and Production of Organic Dairy Cows.” Animals : An Open Access Journal from MDPI, U.S. National Library of Medicine, 18 June 2019, pmc.ncbi.nlm.nih.gov/articles/PMC6617352/.
Zeng, Liuting, et al. “Efficacy and Safety of Curcumin and Curcuma Longa Extract in the Treatment of Arthritis: A Systematic Review and Meta-Analysis of Randomized Controlled Trial.” Frontiers in Immunology, U.S. National Library of Medicine, 22 July 2022, pmc.ncbi.nlm.nih.gov/articles/PMC9353077/.
Stohs, Sidney J, et al. “Highly Bioavailable Forms of Curcumin and Promising Avenues for Curcumin-Based Research and Application: A Review.” Molecules (Basel, Switzerland), U.S. National Library of Medicine, 19 Mar. 2020, pmc.ncbi.nlm.nih.gov/articles/PMC7144558/#:~:text=The%20various%20formulations%20designed%20to,a%20fatty%20meal%20enhances%20absorption.
Intermittent Fasting for IBS Symptoms and Gut Health
With time and consistency, this method can help improve insulin sensitivity (more on this) and improve your body’s ability to use fat stores when glucose is not readily available. Put differently, proper fasting increases metabolism and improves your body’s ability to burn fat.
But there is another physiological benefit of fasting that often gets overlooked - intermittent fasting improves gut health and IBS symptoms.
Fasting to improve gut health
Intermittent fasting benefits are becoming widely known in the weight loss world. But did you know that fasting also has a physiological impact on gut health, and can reduce inflammation and improve microbiome?
Hi friends. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between what their doctor is saying and what their body is saying. Click here to read my Medical Disclaimer.
In this article, you’ll learn:
different types of fasting
physiological effects of fasting
why I recommend fasting for clients with PCOS and IBS symptoms
fasting is not a calorie-counting technique
A common misconception among influencers is that fasting is a great way to get your bod into a calorie deficit. But restricting calories is far from the intention (or physiological impact) of fasting and intermittent fasting.
In fact, calorie restriction has been shown to slow metabolism over time, increase hunger hormones, and decrease satiety hormones [1,2].
Whereas water-fasting and intermittent fasting have been shown to increase growth hormone, improve insulin sensitivity, improve metabolic rate, decrease hunger hormones, and improve your body’s ability to burn fat [3,4,5].
To get a bigger picture of how metabolism works, read this article.
types of fasting
As we’ve discussed, fasting is not merely calorie restriction. What you eat before and after fasting, and the timing and quality of your daily meals, are also important factors when it comes to fasting to improve gut health and insulin resistance.
But let’s talk about different fasting terms first, so you can be on the same page as your health practitioners.
INTERMITTENT FASTING: Also known as Alternate-Day Fasting, refers to a water-only fast for 24-72 hours, with careful attention to refeeding after each fast.
TIME-RESTRICTED FEEDING: Often mistaken for Intermittent Fasting, but the two terms are very different. With Time-Restricted Feeding, one would eat daily, consuming all calories within a set window of time. For example, consuming your calories within an 8-hour period, while fasting the for 16 hours, is commonly known as a “16/8” fast.
EXTENDED FASTING: Water-only fasting that lasts longer than 72 hours.
how fasting works
In a nutshell, when fasting is done well, the intention of fasting is to reduce the amount of insulin being released into your bloodstream by eliminating food intake for a period of time.
With time and consistency, this method can help improve insulin sensitivity (more on this) and improve your body’s ability to use fat stores when glucose is not readily available. Put differently, proper fasting increases metabolism and improves your body’s ability to burn fat.
But there is another physiological benefit of fasting that often gets overlooked - intermittent fasting improves gut health and IBS symptoms.
migrating motor complex
The Migrating Motor Complex (MMC) is the key to repairing IBS symptoms and gut issues associated with PCOS. And it is only active in a fasted state.
That does not mean it cannot occur unless you are doing a 24-hour fast, but it does mean that if you are someone who grazes and snacks throughout the day, your MMC may not be activating much at all.
Here’s why that matters.
The MMC is the body’s mechanism for sweeping out unwanted waste and pathogens from the small intestine. It is a cascade of events that increases motility and digestive enzymes during times of fasting, killing unwanted pathogens and moving them through your digestive tract to the point of elimination.
Something to remember is that digestive function, such as the MMC, cannot occur when you are in fight or flight (sympathetic nervous response). Click here to learn more about how digestion works.
The other side of that coin:
Pathogens like bacteria in the small intestine (SIBO) or candida overgrowth LOVE carbohydrates, and they can cause you to crave these foods, or get excessivley hungry more frequently, so they themselves can get their “food” (carbs).
If the MMC helps to sweep out unwanted pathogens, and certain types of pathogens thrive on the nutrients we eat, it makes sense that fasting improves gut health by essentially starving the gut pathogens (depriving them of nutrients), and increasing activity of the Migrating Motor Complex.
why I recommend intermittent fasting for clients with IBS symptoms and PCOS
In conjunction with addressing digestion and adrenal health, eliminating gut pathogens like candida overgrowth, bacterial overgrowth, and parasites reduces systemic inflammation and can make your IBS symptoms disappear altogether, improve pain levels, and reduce PCOS symptoms.
So cool!
It’s important to remember that eradicating gut pathogens requires a more complex strategy than just implementing intermittent fasting into your routine. But it certainly helps (if your body tolerates it well).
If you want to explore fasting for gut health and IBS symptoms, click here to book a free consultation so we can talk about it.
was this helpful?
Has fasting improved your digestive symptoms and gut health?
Share your thoughts and questions in the comments below!
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
Zauner, C., Schneeweiss, B., Kranz, A., Madl, C., Ratheiser, K., Kramer, L., Roth, E., Schneider, B., & Lenz, K. (2000). Resting energy expenditure in short-term starvation is increased as a result of an increase in serum norepinephrine. The American journal of clinical nutrition, 71(6), 1511–1515. https://doi.org/10.1093/ajcn/71.6.1511
Most, J., & Redman, L. M. (2020). Impact of calorie restriction on energy metabolism in humans. Experimental gerontology, 133, 110875. https://doi.org/10.1016/j.exger.2020.110875
Kolb, Hubert, et al. “Insulin Translates Unfavourable Lifestyle into Obesity - BMC Medicine.” BioMed Central, BioMed Central, 13 Dec. 2018, bmcmedicine.biomedcentral.com/articles/10.1186/s12916-018-1225-1.
Kahn, B. B., & Flier, J. S. (2000). Obesity and insulin resistance. The Journal of clinical investigation, 106(4), 473–481. https://doi.org/10.1172/JCI10842
Fung, J. (2016). The Obesity Code: Unlocking the Secrets of Weight Loss. Greystone Books.
Bowen, Richard. “The Migrating Motor Complex.” Vivo Pathophysiology, Colorado State University, vivo.colostate.edu/hbooks/pathphys/digestion/stomach/mmcomplex.html. Accessed 30 May 2025.